Dagher, R. K., Bruckheim, H. E., Colpe, L. J., Edwards, E. & White, D. B. Perinatal depression: challenges and opportunities. J. Womens Health 30, 154–159 (2021).
Fransson, E., Örtenstrand, A. & Hjelmstedt, A. Antenatal depressive symptoms and preterm birth: a prospective study of a Swedish national sample. Birth 38, 10–16 (2011).
Google Scholar
Iliadis, S. I. et al. Self-harm thoughts postpartum as a marker for long-term morbidity. Front. Public Health 6, 34 (2018).
Google Scholar
Tronick, E. & Reck, C. Infants of depressed mothers. Harvard Rev. Psychiatry 17, 147–156 (2009).
Howard, L. M. et al. Non-psychotic mental disorders in the perinatal period. Lancet 384, 1775–1788 (2014).
Google Scholar
Woody, C. A., Ferrari, A. J., Siskind, D. J., Whiteford, H. A. & Harris, M. G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 219, 86–92 (2017).
Google Scholar
Aziz, H. A., Yahya, H. D. B., Ang, W. W. & Lau, Y. Global prevalence of depression, anxiety, and stress symptoms in different trimesters of pregnancy: a meta-analysis and meta-regression. J. Psychiatr. Res. 181, 528–546 (2025).
Google Scholar
Halbreich, U. & Karkun, S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J. Affect. Disord. 91, 97–111 (2006).
Google Scholar
Josefsson, A., Berg, G., Nordin, C. & Sydsjo, G. Prevalence of depressive symptoms in late pregnancy and postpartum. Acta Obstet. Gynecol. Scand. 80, 251 (2001).
Google Scholar
Rubertsson, C. et al. Depressive symptoms in early pregnancy, two months and one year postpartum-prevalence and psychosocial risk factors in a national Swedish sample. Arch. Womens Ment. Health 8, 97–104 (2005).
Google Scholar
Cox, E. Q., Sowa, N. A., Meltzer-Brody, S. E. & Gaynes, B. N. The perinatal depression treatment cascade: baby steps toward improving outcomes. J. Clin. Psychiatry 77, 20901 (2016).
Altemus, M. et al. Phenotypic differences between pregnancy-onset and postpartum-onset major depressive disorder. J. Clin. Psychiatry 73, 14455 (2012).
Denckla, C. A. et al. Distinguishing postpartum and antepartum depressive trajectories in a large population-based cohort: the impact of exposure to adversity and offspring gender. Psychol. Med. 48, 1139–1147 (2018).
Google Scholar
Wikman, A. et al. Characteristics of women with different perinatal depression trajectories. J. Neurosci. Res. 98, 1268–1282 (2019).
Google Scholar
Bränn, E. et al. Metabolic profiling indicates diversity in the metabolic physiologies associated with maternal postpartum depressive symptoms. Front. Psychiatry 12, 685656 (2021).
Google Scholar
Diagnostic and Statistical Manual of Mental Disorders 5th edn (APA, 2013).
Aldao, A., Nolen-Hoeksema, S. & Schweizer, S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 30, 217–237 (2010).
Google Scholar
Gratz, K. L. & Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 26, 41–54 (2004).
Rammensee, R. A., Morawetz, C., & Basten, U. Individual differences in emotion regulation: personal tendency in strategy selection is related to implementation capacity and well-being. Emotion (2023).
McRae, K., Misra, S., Prasad, A. K., Pereira, S. C. & Gross, J. J. Bottom-up and top-down emotion generation: implications for emotion regulation. Soc. Cogn. Affect. Neurosci. 7, 253–262 (2012).
Google Scholar
Sheppes, G., Suri, G. & Gross, J. J. Emotion regulation and psychopathology. Annu. Rev. Clin. Psychol. 11, 379–405 (2015).
Google Scholar
Radke, S. et al. Imaging the up’s and down’s of emotion regulation in lifetime depression. Brain Imaging Behav. 12, 156–167 (2018).
Google Scholar
D’Agostino, A., Covanti, S., Rossi Monti, M. & Starcevic, V. Reconsidering emotion dysregulation. Psychiatr. Q. 88, 807–825 (2017).
Google Scholar
Gingnell, M. et al. Emotion reactivity is increased 4–6 weeks postpartum in healthy women: a longitudinal fMRI study. PLoS ONE 10, e0128964 (2015).
Google Scholar
McDonald, H. M., Sherman, K. A. & Kasparian, N. A. A mediated model of mindful awareness, emotion regulation, and maternal mental health during pregnancy and postpartum. Aust. J. Psychol. 73, 368–380 (2021).
Penner, F., Bunderson, M., Bartz, C., Brooker, R. J. & Rutherford, H. J. Emotion regulation strategies and perceived stress during pregnancy in expectant mothers and fathers. J. Reprod. Infant Psychol. 42, 410–423 (2022).
Google Scholar
Penner, F. & Rutherford, H. J. Emotion regulation during pregnancy: a call to action for increased research, screening, and intervention. Arch. Womens Ment. Health 25, 527–531 (2022).
Google Scholar
Conradt, E. et al. Prenatal maternal hair cortisol concentrations are related to maternal prenatal emotion dysregulation but not neurodevelopmental or birth outcomes. Dev. Psychobiol. 62, 758–767 (2020).
Google Scholar
Kalmbach, D. A. et al. Mindfulness and nocturnal rumination are independently associated with symptoms of insomnia and depression during pregnancy. Sleep Health 6, 185–191 (2020).
Google Scholar
Bradizza, C. M. et al. Smoking cessation for pregnant smokers: development and pilot test of an emotion regulation treatment supplement to standard smoking cessation for negative affect smokers. Nicotine Tob. Res. 19, 578–584 (2017).
Google Scholar
Lin, B. et al. Intergenerational transmission of emotion dysregulation: part I. Psychopathology, self-injury, and parasympathetic responsivity among pregnant women. Dev. Psychopathol. 31, 817–831 (2019).
Google Scholar
Coo, S., García, M. I., Prieto, F. & Medina, F. The role of interpersonal emotional regulation on maternal mental health. J. Reprod. Infant Psychol. 40, 3–21 (2022).
Google Scholar
Marques, R., Monteiro, F., Canavarro, M. C. & Fonseca, A. The role of emotion regulation difficulties in the relationship between attachment representations and depressive and anxiety symptoms in the postpartum period. J. Affect. Disord. 238, 39–46 (2018).
Google Scholar
Paley, B. & Hajal, N. J. Conceptualizing emotion regulation and coregulation as family-level phenomena. Clin. Child Fam. Psychol. Rev. 25, 19–43 (2022).
Google Scholar
Barrett, E. N., et al. Psychometric properties of the Difficulties in Emotion Regulation Scale in a perinatal sample. J. Reprod. Infant Psychol. (2023).
Goldstein, B. L., Briggs-Gowan, M. J., Greene, C. C., Chang, R. & Grasso, D. J. An Item Response Theory examination of the original and short forms of the Difficulties in Emotion Regulation Scale (DERS) in pregnant women. J. Clin. Psychol. 77, 1591–1606 (2021).
Google Scholar
Hallion, L. S., Steinman, S. A., Tolin, D. F. & Diefenbach, G. J. Psychometric properties of the Difficulties in Emotion Regulation Scale (DERS) and its short forms in adults with emotional disorders. Front. Psychol. 9, 539 (2018).
Google Scholar
Bjureberg, J. et al. Development and validation of a brief version of the difficulties in emotion regulation scale: the DERS-16. J. Psychopathol. Behav. Assess. 38, 284–296 (2016).
Google Scholar
Hajal, N. J. & Paley, B. Parental emotion and emotion regulation: a critical target of study for research and intervention to promote child emotion socialization. Dev. Psychol. 56, 403 (2020).
Google Scholar
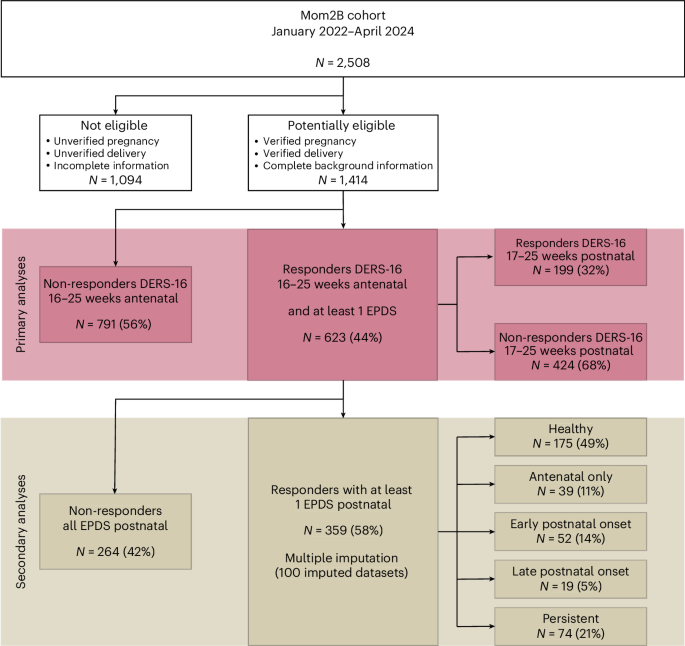
Bilal, A. M. et al. Protocol: predicting perinatal health outcomes using smartphone-based digital phenotyping and machine learning in a prospective Swedish cohort (Mom2B): study protocol. BMJ Open (2022).
Sacher, J., Chechko, N., Dannlowski, U., Walter, M. & Derntl, B. The peripartum human brain: current understanding and future perspectives. Front. Neuroendocrinol. 59, 100859 (2020).
Google Scholar
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150, 782–786 (1987).
Google Scholar
Rubertsson, C., Börjesson, K., Berglund, A., Josefsson, A. & Sydsjö, G. The Swedish validation of Edinburgh Postnatal Depression Scale (EPDS) during pregnancy. Nord. J. Psychiatry 65, 414–418 (2011).
Google Scholar
Wickberg, B. & Hwang, C. P. The Edinburgh Postnatal Depression Scale: validation on a Swedish community sample. Acta Psychiatr. Scand. 94, 181–184 (1996).
Google Scholar
Lincoln, T. M., Schulze, L. & Renneberg, B. The role of emotion regulation in the characterization, development and treatment of psychopathology. Nat. Rev. Psychol. 1, 272–286 (2022).
Haga, S. M. et al. A longitudinal study of postpartum depressive symptoms: multilevel growth curve analyses of emotion regulation strategies, breastfeeding self-efficacy, and social support. Arch. Womens Ment. Health 15, 175–184 (2012).
Google Scholar
Ifeagwazi, C. M., Obiajulu, B. M., Chukwuorji, J. C. & Ndukaihe, I. L. Emotion dysregulation robustly predicts depressive symptoms above and beyond life events and social support in sub-Saharan African pregnant women. Womens Reprod. Health 8, 29–43 (2021).
International Classification of Diseases (ICD) 11th edn (WHO, 2022); https://www.who.int/classifications/icd/en/.
D’Avanzato, C., Joormann, J., Siemer, M. & Gotlib, I. H. Emotion regulation in depression and anxiety: examining diagnostic specificity and stability of strategy use. Cogn. Ther. Res. 37, 968–980 (2013).
Hervás, G. & Jódar, R. Adaptación al castellano de la Escala de Dificultades en la Regulación Emocional. Clín. salud 19, 139–156 (2008).
Falah-Hassani, K., Shiri, R., Vigod, S. & Dennis, C. L. Prevalence of postpartum depression among immigrant women: a systematic review and meta-analysis. J. Psychiatr. Res. 70, 67–82 (2015).
Google Scholar
Goldberg, S. B., Bolt, D. M. & Davidson, R. J. Data missing not at random in mobile health research: assessment of the problem and a case for sensitivity analyses. J. Med. Internet Res. 23, e26749 (2021).
Google Scholar
Judd, F., Lorimer, S., Thomson, R. H. & Hay, A. Screening for depression with the Edinburgh Postnatal Depression Scale and finding borderline personality disorder. Aust. N. Z. J. Psychiatry 53, 424–432 (2019).
Google Scholar
Lautarescu, A. et al. The factor structure of the Edinburgh Postnatal Depression Scale among perinatal high-risk and community samples in London. Arch. Womens Ment. Health (2022)
Rondung, E. et al. Identification of depression and anxiety during pregnancy: a systematic review and meta-analysis of test accuracy. Acta Obstet. Gynecol. Scand. 103, 423–436 (2024).
Google Scholar
Bloch, M., Rotenberg, N., Koren, D. & Klein, E. Risk factors associated with the development of postpartum mood disorders. J. Affect. Disord. 88, 9–18 (2005).
Google Scholar
Giallo, R. et al. Physical, sexual and social health factors associated with the trajectories of maternal depressive symptoms from pregnancy to 4 years postpartum. Soc. Psychiatry Psychiatr. Epidemiol. 52, 815–828 (2017).
Google Scholar
Larsen, S. V., Mikkelsen, A. P., Lidegaard, Ø & Frokjaer, V. G. Depression associated with hormonal contraceptive use as a risk indicator for postpartum depression. JAMA Psychiatry 80, 682–689 (2023).
Google Scholar
Agako, A. et al. The role of emotion dysregulation in cognitive behavioural group therapy for perinatal anxiety: results from a randomized controlled trial and routine clinical care. J. Affect. Disord. 292, 517–525 (2021).
Google Scholar
Agako, A. et al. A pilot study examining the effectiveness of a short-term, DBT informed, skills group for emotion dysregulation during the perinatal period. Psychol. Serv. 20, 697 (2023).
Google Scholar
Deogan, C., Abrahamsson, K., Mannheimer, L. & Björkenstam, C. Having a child without wanting to? Estimates and contributing factors from a population-based survey in Sweden. Scand. J. Public Health 50, 215–222 (2022).
Google Scholar
Kopp Kallner, H., Thunell, L., Brynhildsen, J., Lindeberg, M. & Gemzell Danielsson, K. Use of contraception and attitudes towards contraceptive use in Swedish women—a nationwide survey. PLoS ONE 10, e0125990 (2015).
Google Scholar
Andersson, S., Bathula, D. R., Iliadis, S. I., Walter, M. & Skalkidou, A. Predicting women with depressive symptoms postpartum with machine learning methods. Sci. Rep. 11, 7877 (2021).
Google Scholar
Hildingsson, I., Rubertsson, C., Karlström, A. & Haines, H. Exploring the Fear of Birth Scale in a mixed population of women of childbearing age—a Swedish pilot study. Women Birth 31, 407–413 (2018).
Google Scholar
Aiena, B. J., Baczwaski, B. J., Schulenberg, S. E. & Buchanan, E. M. Measuring resilience with the RS–14: a tale of two samples. J. Pers. Assess. 97, 291–300 (2015).
Google Scholar
Wagnild, G. M. & Young, H. M. Development and psychometric evaluation of the resilience scale. J. Nurs. Meas. 1, 165–178 (1993).
Google Scholar
Antonovsky, A. The structure and properties of the sense of coherence scale. Soc. Sci. Med. 36, 725–733 (1993).
Google Scholar
Eriksson, M. & Lindström, B. Validity of Antonovsky’s sense of coherence scale: a systematic review. J. Epidemiol. Community Health 59, 460–466 (2005).
Google Scholar
Boyce, P., Hickey, A., Gilchrist, J. & Talley, N. J. The development of a brief personality scale to measure vulnerability to postnatal depression. Arch. Womens Ment. Health 3, 147–153 (2001).
Dennis, C. L. & Boyce, P. Further psychometric testing of a brief personality scale to measure vulnerability to postpartum depression. J. Psychosom. Obstet. Gynaecol. 25, 305–311 (2004).
Google Scholar
Hajure, M. et al. Resilience and mental health among perinatal women: a systematic review. Front. Psychiatry 15, 1373083 (2024).
Google Scholar
Pollock, N. C., McCabe, G. A., Southard, A. C. & Zeigler-Hill, V. Pathological personality traits and emotion regulation difficulties. Pers. Individ. Dif. 95, 168–177 (2016).
Rufino, K. A., Babb, S. J. & Johnson, R. M. Moderating effects of emotion regulation difficulties and resilience on students’ mental health and well-being during the COVID-19 pandemic. J. Adult Contin. Educ. 28, 397–413 (2022).
van Buuren S. & Groothuis-Oudshoorn, K. mice: multivariate imputation by chained equations in R. J. Stat. Softw. (2011).
link






